In 2018, the U.S. heart transplant allocation system was modified with the goal of improving access to heart transplants. This brief examines the impact of this policy change on equity in transplant access among patients at the greatest risk of pre-transplant death.
Examining Equity in Access to Heart Transplantation After 2018 Policy Change
In October 2018, the United States National Organ Procurement Transplant Network/United Network for Organ Sharing (OPTN/UNOS) modified the heart transplant allocation system for adults as part of a strategic goal to provide equity in access to transplants.1 The goal was to enable more heart transplants for the people who need them the most, with the same likelihood of receiving a transplant regardless of patients’ socioeconomic status and location.
More specifically, UNOS revised the heart allocation system to improve access for those at greatest risk of pre-transplant death, such as patients who receive short-term mechanical circulatory support (MCS). The revision was intended to reduce waitlist mortality. Experts agree that short-term MCS should be reserved for patients with the most severe heart failure for whom the benefits exceed the risks, but as using this therapy is a clinical judgment, variation between clinicians and centers is expected. However, equitable access to heart transplants could be impacted if individual centers substantially differ in decisions and clinical judgment related to patient selection for short-term MCS use.
A University of Michigan research team studied this issue using the OPTN/UNOS database to compare the 12 months before and after implementation of the October 2018 policy change among 5,477 adult heart transplant recipients. The team looked at: 1) if there was a change in the use of short-term MCS overall and 2) if there was an increase in center-level variation in the use of short-term MCS after the heart allocation system update.
Short-term mechanical circulatory support (MCS) devices are heart pumps that are meant to support the failing heart for a limited time — generally less than a week. This invasive therapy helps provide blood to vital organs that the heart is unable to supply but can result in major complications.
Takeaways from our research*

1. 143 heart transplant centers performed over 2,700 transplants per year in the year before and after implementation of the new transplant allocation system.

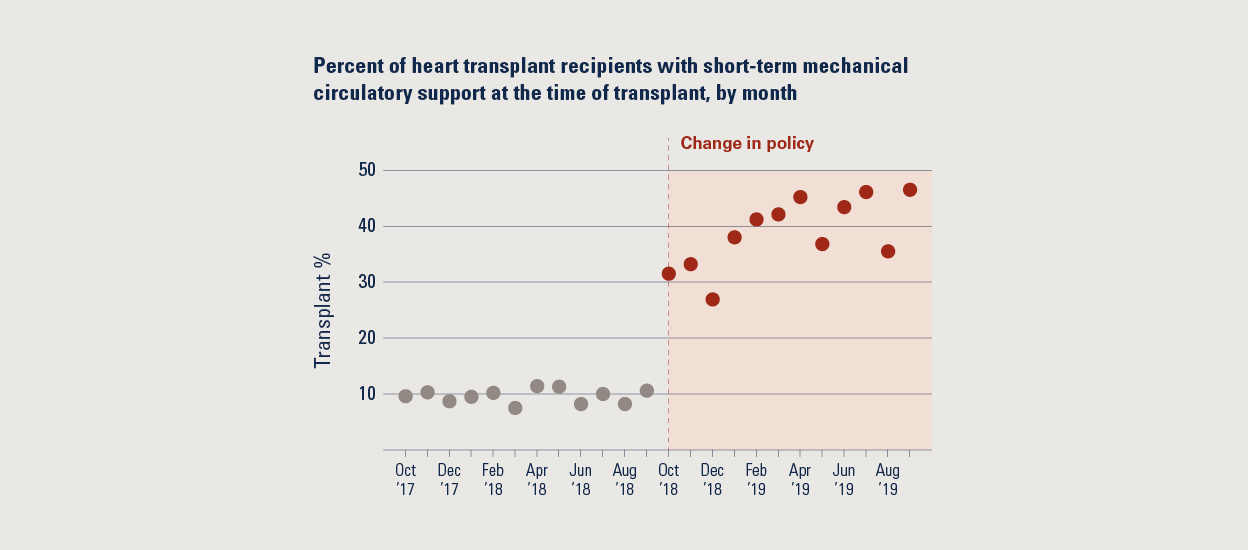
2. Short-term MCS use increased by 23% at the time of heart transplant immediately following the 2018 policy change. This initial increase was sustained and continued to expand each month in the following year. These findings suggest that clinicians have responded to the revised allocation system with evolving changes in clinical practice, raising concern that some of the increased short-term MCS use may be for patients whose needs are less urgent.
3. The rise in use of short-term MCS was not consistent across transplant centers. The increased variation in practice patterns leads to unfair access to transplants for some patients, depending on where they received care.
What does this mean for health policy and practice?
These study findings suggest there is a need to continue to modify the heart transplant allocation system in order to meet the strategic goal of promoting equity in access.
UNOS policymakers could consider:
- Tracking the impact of center-level variation in practice on equity.
- The recently released Equity in Access to Transplant Dashboard is being used by OPTN to monitor system-level trends.2 Given the wide variability in practice between centers, this dashboard could include metrics to track center-level variation, with considerations for repercussions for misuse.
- Increasing collaboration between centers.
- Dissemination of best practice case discussions.
- Regular listing meetings between rotating groups of centers to encourage greater uniformity of practice.
- Developing and adopting risk scores that do not include therapies as a surrogate for illness severity.
- The use of therapies such as short-term MCS is based on a clinician’s judgment and differs between centers. There would be less variability if risk scores were based on objective criteria such as age and kidney function as determined by labs.
- Establishing more stringent criteria to justify the health status level of patients who receive short-term MCS.
- Currently, the criteria, such as low blood pressure and a decreased amount of blood being pumped by the heart, are at levels that are frequently seen in patients who do not require emergent, life-saving therapies.
REFERENCED STUDY
*Cascino, Thomas M. et al. A challenge to equity in transplantation: Increased center-level variation in short-term mechanical circulatory support use in the context of the updated U.S. heart transplant allocation policy. The Journal of Heart and Lung Transplantation. In Press Journal Pre-Proof Published online: September 15, 2021. https://www.jhltonline.org/article/S1053-2498(21)02494-3/fulltext
REFERENCES
1 Modify Adult Heart Allocation 2016 2nd round. Organ Procurement and Transplantation Network. Accessed July 11, 2020. https://optn.transplant.hrsa.gov/governance/public-comment/modify-adult-heart-allocation-2016-2nd-round/.
2 Equity in Access to Transplant. Organ Procurement and Transplantation Network. Accessed July 15, 2021. https://insights.unos.org/equity-in-access/.
AUTHORS
Thomas M. Cascino, MD, MSc1,7; Josef Stehlik, MD, MPH2; Wida Cherikh, PhD3; Donald S. Likosky, PhD4,7; Keith D. Aaronson, MD, MS1
CONTRIBUTORS
Yulin Cheng, BS3; Tessa M. F. Watt, MD MSc4; Alexander A. Brescia, MD, MSc4; Michael P. Thompson, PhD4,7; Jeffrey S. McCullough, PhD5,7; Min Zhang, PhD6,7; Supriya Shore, MD, MSc1,7; Jessica Golbus, MD, MS4; Francis D. Pagani, MD, PhD4,7; on behalf of the Michigan Congestive Heart Failure Investigators.
1 Division of Cardiovascular Medicine, Medical School, University of Michigan; 2 Division of Cardiovascular Medicine, University of Utah, Salt Lake City, UT; 3 United Network for Organ Sharing, Richmond, VA; 4 Department of Cardiac Surgery, Medical School, University of Michigan; 5 Department of Health Management and Policy, School of Public Health, University of Michigan; 6 Department of Biostatistics, School of Public Health, University of Michigan, 7 Institute for Healthcare Policy & Innovation, University of Michigan
ACKNOWLEDGMENTS
This policy brief was supported by the IHPI Policy Sprint program, which provides funding and staff assistance to IHPI member-led teams in undertaking rapid analyses to address important health policy questions and develop products that inform decision-making at the local, state, or national level.
FOR MORE INFORMATION
Please contact Eileen Kostanecki, IHPI’s Director of Policy Engagement & External Relations, at [email protected].
