U-M researchers analyze the relationship between virtual care adoption among primary care practices and emergency department visits or hospitalizations amid the COVID-19 pandemic.
Telehealth Use in Michigan During COVID-19
Variation in Primary Care Telehealth Adoption and Its Impact on Emergency Department Use and Hospitalizations
 Prior to the COVID-19 public health emergency, telehealth use in primary care was rare. During the early surge of COVID-19, in-person services were discouraged to prevent the spread of infection and conserve personal protective equipment. A state of Michigan Executive Order suspended all non-essential medical and dental visits from March 21–May 29, 2020.1 The pandemic spurred a number of policy and regulatory changes that led to rapid expansion of telehealth services to provide access to care.
Prior to the COVID-19 public health emergency, telehealth use in primary care was rare. During the early surge of COVID-19, in-person services were discouraged to prevent the spread of infection and conserve personal protective equipment. A state of Michigan Executive Order suspended all non-essential medical and dental visits from March 21–May 29, 2020.1 The pandemic spurred a number of policy and regulatory changes that led to rapid expansion of telehealth services to provide access to care.
Limited access to primary care can lead to worse control of ambulatory care sensitive conditions (ACSCs) and preventable emergency department visits or hospitalizations. The impact of rising telehealth use on healthcare utilization and spending for these conditions was unknown.
Ambulatory Care Sensitive Conditions (ACSCs) are “conditions for which good outpatient care can potentially prevent the need for hospitalization, or for which early intervention can prevent complications or more severe disease." 2 Medicare payments to primary care practices have previously been tied to their performance on these measures.3
Acute ACSCs include conditions such as dehydration, urinary tract infection, and pneumonia.
Chronic ACSCs include exacerbations of congestive heart failure, chronic obstructive pulmonary disease, and complications of diabetes.
Takeaways from our study
A team at the University of Michigan used claims data from a major commercial insurer, Blue Cross Blue Shield of Michigan, to determine differences in telehealth adoption across over 4,000 primary care practices in Michigan and study the relationship between telehealth adoption levels and emergency department (ED) visits or hospitalizations for ACSCs. The overall study period was March–September 2020. The dataset included claims for visits for children and adults.
1. Telehealth only partially offset the decline in access to primary care in the first few months of the pandemic
Telehealth use rapidly expanded during the first COVID-19 wave in Michigan, making up 59% of primary care visits at its peak in April 2020 and plateauing in the following months.
Despite the rise in the use of telehealth, the number of primary care visits declined sharply from March to May 2020. Total visits fell to as low as 47% of the number of visits in the same period in 2019.
2. Telehealth adoption among primary care practices varied widely in Michigan
Most primary care practices (71%) used some degree of telehealth during the pandemic, but this varied by practice size and urbanicity.
- Percent of primary care practices that used some degree of telehealth
- 63% Solo practices
- 91% Large practices of more than 20 providers
- 61% Rural areas
- 73% Urban areas
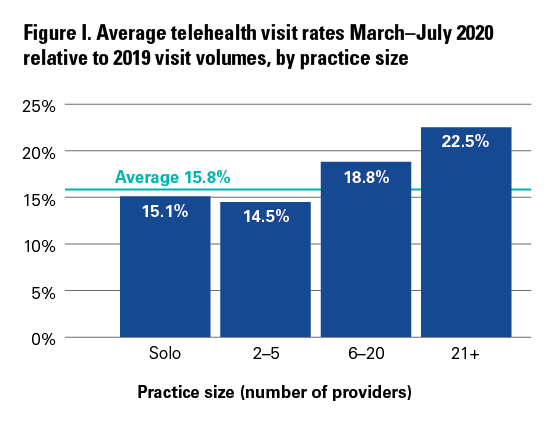
In addition to being more likely to use telehealth at all, larger practices performed a greater share of their visits by telehealth than smaller practices. See figure I below.
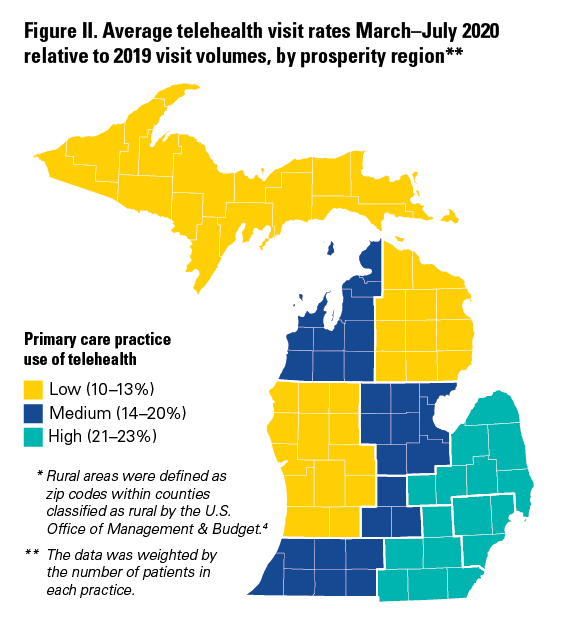
More rural areas in Northern and Western regions of the state were less likely to adopt telehealth than more urban and suburban regions in the Southeast.* See figure II below.
3. There was no strong relationship between primary care practice telehealth use and emergency department (ED) visits and hospitalizations for ACSCs
1. Overall, the rate of ED visits and hospitalizations for ACSCs declined sharply in March–April 2020. The rate of visits then increased and plateaued in subsequent months, still remaining below pre-pandemic levels.
- Visit trends were similar for both acute and chronic ACSCs during this timeframe.
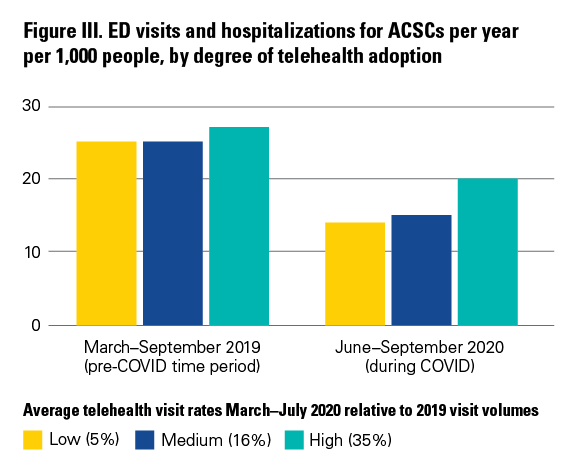
2. The difference in ED visit or hospitalization rates between the highest and lowest telehealth adopters was marginal.
- Practices with the greatest proportion of visits converted to telehealth had slightly higher rates of visits for ACSCs (an increase of 1 to 2 visits per year per 1,000 people for acute and chronic ACSCs, respectively).
3. There was no difference in ED visit or hospitalization rates between practices that did a moderate amount of telehealth and very little or no telehealth.
Conclusions and implications for policy and practice
While telehealth use rapidly expanded in 2020, smaller and rural practices were lagging, potentially worsening disparities in a large portion of the state. While prior data shows lower rates of telehealth use among patients in rural areas compared to patients in urban areas5, this study suggests that rural primary care providers may also face barriers to adoption.
Although practices that used more telehealth during the early months of the COVID-19 pandemic experienced marginally higher rates of ED visits and hospitalizations for ACSCs, this period of time coincided with a period of unprecedented fluctuations in care utilization in Michigan and across the country. Nevertheless, this early look shows that the impact of telehealth on downstream hospitalizations and emergency room visits may not be as large as either proponents or critics of telehealth have suggested. The relationship between telehealth use and visits for ACSCs is complex and merits continued research.
REFERENCES
1. Executive Order 2020–17: Temporary Restrictions on Non-Essential Medical and Dental Procedures; 2020. Accessed February 12, 2021. https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-522451--,00.html.
2. Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Agency for Healthcare Research and Quality. Accessed October 13, 2020. https://www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf.
3. 2016 Measure Information About the Hospital Admissions for Acute and Chronic Ambulatory Care Condition (ACSC) Composite Measures, Calculated for the 2018 Value-Based Payment Modifier Program. Centers for Medicare and Medicaid Services. Accessed October 14, 2020. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Downloads/2016-ACSC-MIF.pdf.
4. Defining Rural Population. Federal Office of Rural Health Policy. Accessed March 4, 2021. https://www.hrsa.gov/rural-health/about-us/definition/index.html.
5. Rural Individuals’ Telehealth Practices: An Overview, EIB-199. Stenberg, PL. U.S. Department of Agriculture, Economic Research Service. Accessed March 9, 2021. https://www.ers.usda.gov/webdocs/publications/90530/eib-199.pdf?v=869.3.
AUTHORS
Kathleen Y. Li, MD, MS1,2
Sophia Ng, PhD2
Jeff McCullough, PhD2,3
Ziwei Zhu, MS4
Keith Kocher, MD, MPH1,2
Chad Ellimoottil, MD, MS2,4
1 Department of Emergency Medicine, 2 Institute for Healthcare Policy and Innovation, 3 Health Management and Policy, 4 Department of Urology, all at the University of Michigan.
ACKNOWLEDGMENTS
This policy brief was supported by the IHPI Policy Sprint program, which provides funding and staff assistance to IHPI member-led teams in undertaking rapid analyses to address important health policy questions and develop products that inform decision-making at the local, state, or national level.
FOR MORE INFORMATION
Please contact Eileen Kostanecki, IHPI’s Director of Policy Engagement & External Relations, at [email protected].
