As telehealth use surged during the COVID-19 pandemic, understanding its use for outpatient evaluation and the extent it continues to serve as a substitute for in-person care are important analyses. This brief examines national Medicare claims data to better understand whether the use of telehealth led to an increase in the overall volume of outpatient evaluation and management services delivered to Medicare beneficiaries.
An evaluation of telehealth use by Medicare beneficiaries in 2020
At the start of the COVID-19 public health emergency, the federal government made temporary Medicare policy changes to expand telehealth coverage, resulting in a surge in telehealth use for outpatient evaluation and management (E&M) services.1,2 Early in the pandemic, telehealth was a necessary substitute for in-person care; however, the extent to which telehealth continues to serve as a substitute for in-person care, as opposed to being a complement to care, is not clear. As federal and state policymakers consider policy options to permanently expand telehealth, it is important to understand whether the use of telehealth has led to an increase in the overall volume of E&M services being delivered to Medicare beneficiaries.
Outpatient Evaluation and Management (E&M) Services include new and established patient office visits, psychotherapy visits, wellness visits
Telehealth services include video visits, phone visits, virtual check-ins, online digital evaluations, interprofessional consultations, and remote monitoring
Telehealth users in this study are Medicare beneficiaries who received at least one outpatient telehealth service in 2019 or 2020
Telehealth non-users in this study are Medicare beneficiaries who did not receive any telehealth services in 2019 or 2020
Takeaways from our study
A team at the University of Michigan used national Medicare claims data to examine how telehealth use for outpatient evaluation and management (E&M) services changed during the course of the coronavirus pandemic. The study period was January 2019-December 2020. The dataset included claims from a 20% national random sample of fee-for-service Medicare beneficiaries during the study period.
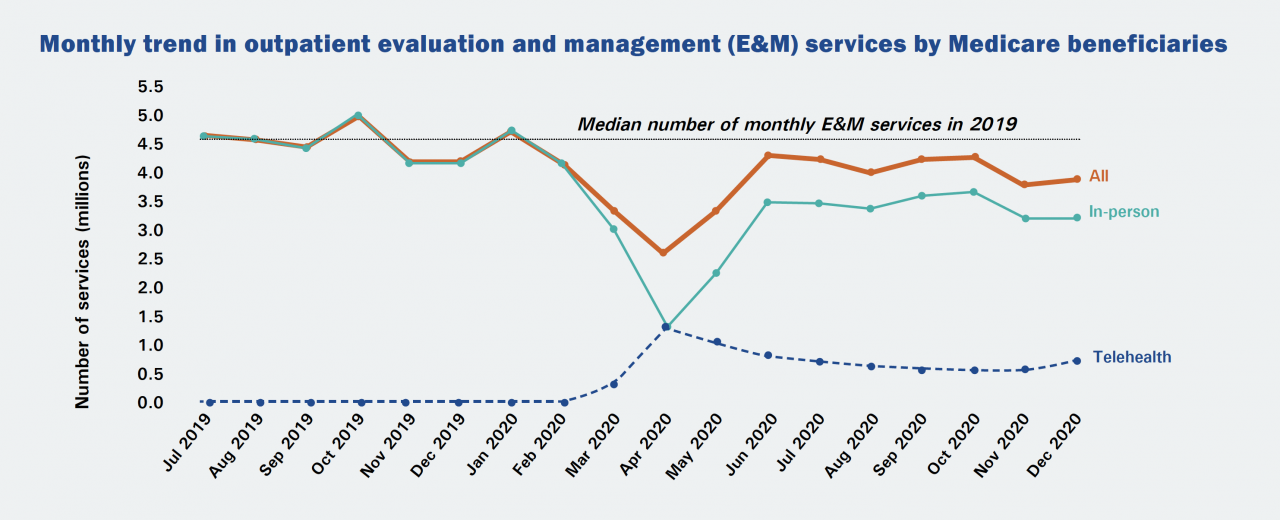
1. Telehealth use surged during the early months of the coronavirus pandemic and then plateaued through the end of December 2020.
- Telehealth services made up 0.2% of all outpatient E&M services in February 2020 and reached a peak of 50.7% in April 2020.
- From July 2020 through December 2020, monthly rates of telehealth ranged from 13.5% to 18.3%.
2. Beyond the early part of the coronavirus pandemic, telehealth continues to be used as a substitute for in-person care.
- The combined number of monthly telehealth and in-person services in 2020 has not exceeded the median number of monthly E&M services in 2019, suggesting that telehealth has been used primarily as a substitute for in-person care.
3. Rural beneficiaries used a disproportionately lower level of telehealth services compared to non-rural beneficiaries.
- 44% percent of all Medicare beneficiaries received at least one telehealth service during the study period.
- A lower percent of rural residents are telehealth users compared to those who live in non-rural zip codes (34% vs 47%).
Conclusions and implications for policy
Our findings mitigate some concerns that telehealth expansion will increase the overall use of services.
- While telehealth use surged during the early months of the coronavirus pandemic, it then plateaued through the end of December 2020.
- So far, the increase in telehealth has not led to an increase in the overall volume of E&M services, suggesting that telehealth is still being used as a substitute for in-person care. However, some patients may be avoiding all care.
Importance of policies geared towards advancing telehealth capabilities in rural areas.
- Rural beneficiaries used a disproportionately lower level of telehealth services compared to non-rural beneficiaries.
- Because rural beneficiaries might stand to benefit the most from telehealth, policymakers could focus on improving rural access to telehealth by exploring rural usage and desire to use telehealth.
REFERENCES
1 Medicare Payment Advisory Commission.March 2021 Report to the Congress: Medicare Payment Policy.; 2021. http://www.medpac.gov/docs/default-source/reports/mar21_medpac_report_ch14_sec.pdf?sfvrsn=0.
2 Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19. Accessed July 24, 2021. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/.
AUTHORS
Chad Ellimoottil, MD, MS1,3; Ziwei Zhu, MS1; Rod Dunn, MS1; Ganesh Palapattu, MD1,4; David Miller, MD, MPH1,3; Andrew M. Ryan, PhD3; Michael P. Thompson, PhD2,3
1 Department of Urology, University of Michigan, Ann Arbor; 2 Department of Cardiac Surgery, University of Michigan, Ann Arbor; 3 University of Michigan Institute for Healthcare Policy & Innovation, Ann Arbor; 4 Department of Urology, Medical University of Vienna, Vienna Austria
ACKNOWLEDGMENTS
Sophia Ng, PhD for her review of our statistical code and manuscript
Dr. Ellimoottil is funded by Agency for Healthcare Research and Quality (AHRQ) through 1 K08 HS027632-01
FOR MORE INFORMATION
Please contact Eileen Kostanecki, IHPI’s Director of Policy Engagement & External Relations, at [email protected].