Study: Cost and Weight-Loss Potential Matter Most to Bariatric Surgery Patients
A survey examines what qualities patients look for when choosing a bariatric surgery procedure. But those needs might not align with their final decision.
Imagine you are picking a weight loss procedure today.
Depending on your age, some aspects of surgery will matter more than others. But the main concerns on people’s minds, a new study at Michigan Medicine has found, are cost and how much weight they can lose — not risk of complications or recovery time.
That thinking process guided a new study published in JAMA Surgery, which sought to explore how bariatric surgery recipients make decisions and process complex information.
“Instead of asking patients about the reasons for or against particular procedures, we asked patients to tell us what procedure characteristics mattered to them the most,” says lead author Michael Rozier, Ph.D., who studied health care management and policy at the University of Michigan.
Rozier partnered with senior author Lisa Prosser, Ph.D., professor of pediatrics at the U-M Medical School and member of U-M Institute for Healthcare Policy and Innovation, for a unique application of marketing principles to gain insight on health care choices.
As director of the U-M’s Child Health Evaluation and Research Center, Prosser says conjoint analysis which has been used to understand consumer preferences before products hit the market has helped gain insight on how people decide on vaccinations, newborn screening and other health choices.
In this case, it helped researchers learn what aspects of bariatric surgery patients value.
And the results were surprising: the most commonly performed bariatric surgery, sleeve gastrectomy, doesn’t fit the top qualities that surveyed patients want out of their weight loss journey.
Compared to gastric bypass, patients who have sleeve gastrectomy lose less weight, on average during the first year.
What bariatric surgery patients want
People with obesity have numerous options to consider when looking for the approach that works best for them
For those seeking a surgical solution, finding the right treatment can be as complex as the condition itself, according to the Patient-Centered Outcomes Research Institute, an independent nonprofit that funded the study.
Nationwide, 93 million adults and 1 in 5 adolescents are obese. They’re at greater risk for heart disease, type 2 diabetes and cancer, among other health problems.
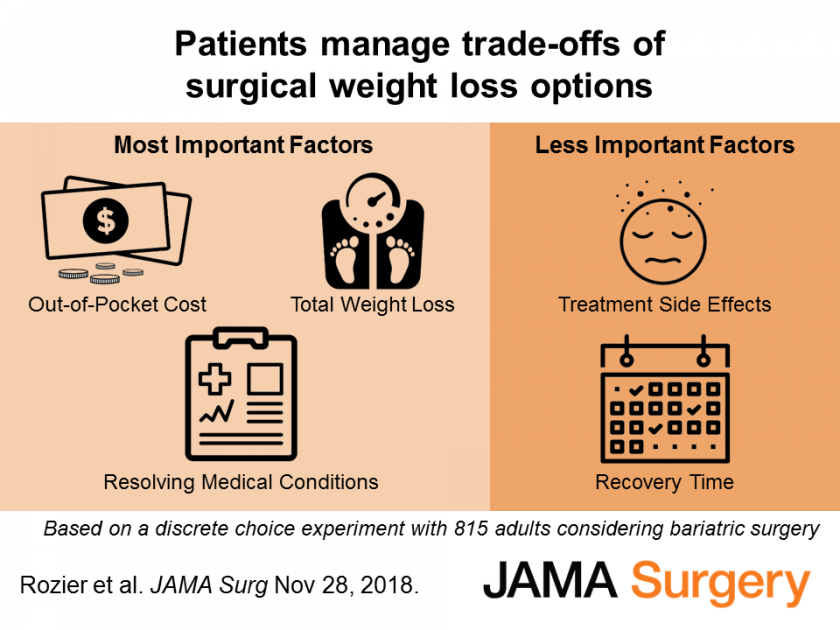
The JAMA Surgery study found that these patients were likely to base their weight loss surgery choice on expected out-of-pocket costs, weight-loss potential and resolution of medical conditions.
They appeared less influenced by a procedure’s related risks.
More than 800 adults revealed their preferences in the analysis performed at Michigan Medicine, U-M’s academic medical center. Participants were recruited for the online survey from bariatric surgery information sessions around the state.
A patient’s gender also appeared to play a role. Men were more likely than women to say they wanted a weight loss surgery that could help them stop taking medication to control high blood pressure, blood sugar and cholesterol, and to achieve remission of obesity-related sleep apnea.
Preferences buck surgical trends
Based on stated preferences revealed in the survey, more people would ideally receive gastric bypass surgery — in which the stomach is turned into a tiny pouch and the intestines rerouted.
In real-life practice, however, sleeve gastrectomy has taken off nationally and internationally as the most common operation for obesity.
This involves about 80 percent of the stomach being removed, greatly reducing its storage capacity and, as a result, limiting production of the hunger-producing hormone ghrelin. Sleeve gastrectomy is known for being a less technically demanding operation with potentially fewer long-term complications.
Still, each option has pros and cons.
“We know there may be slightly better weight loss and increased comorbidity resolution with bypass, so recommending sleeve gastrectomy may be somewhat different than what patients in this study valued,” says study co-author Amir Ghaferi, M.D., M.S., a bariatric surgeon at Michigan Medicine and director of the Michigan Bariatric Surgery Collaborative.
The unique data is “important in guiding conversations and expectations,” says Ghaferi who does health services research as a member of U-M IHPI. Those discussions may include coming to terms with the potential for weight regain in the years after bariatric surgery.
Data collected in the study helped with development of the patient guide My Weight Loss Journey, which looks at surgery risks and benefits. The online decider tool helps users select a bariatric surgery based on side effects and the type of diet that must be followed afterwards.
The team is set to embark on an additional study to gain surgeon responses to the same survey.
“The new data may help providers understand where their intuition might be different from what patients want,” says Prosser.
Weighing in on money issues
The survey’s findings on financial concerns underscore an existing gap: Health care providers are rarely trained how to discuss the out-of-pocket costs of given procedures with their patients.
“In fact, we often discourage providers from entering into that area of conversation because we don’t want money to influence the relationship between providers and patients,” says Rozier, now an assistant professor of health management and policy at the Saint Louis University College for Public Health and Social Justice.
But it matters, he says, especially among patients ages 18 to 44.
“Our results show it matters a great deal to patients,” Rozier says. “So we probably need to figure out an appropriate way to incorporate cost into conversations providers have with their patients.”

