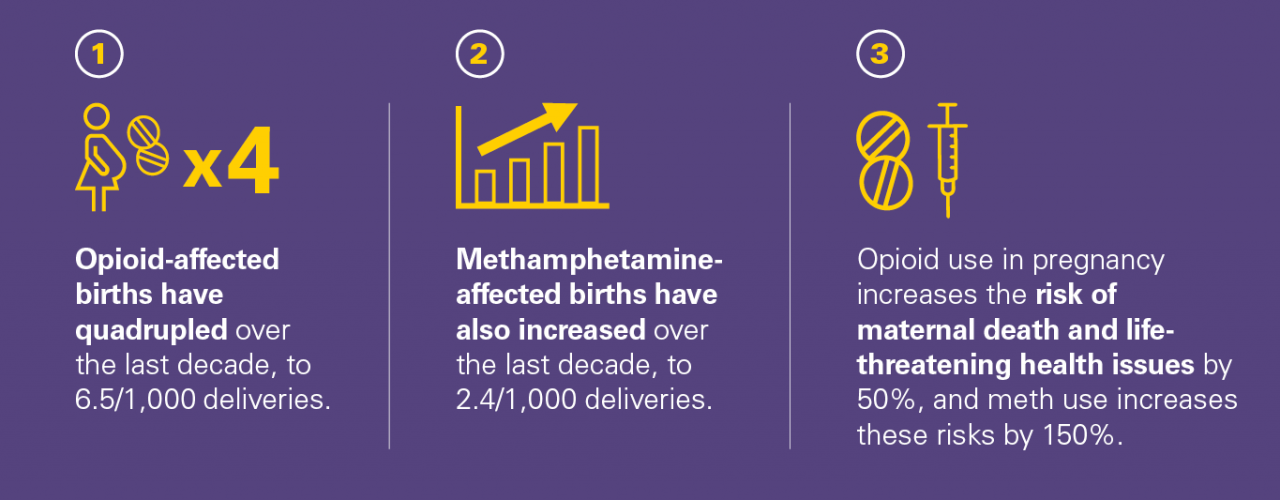
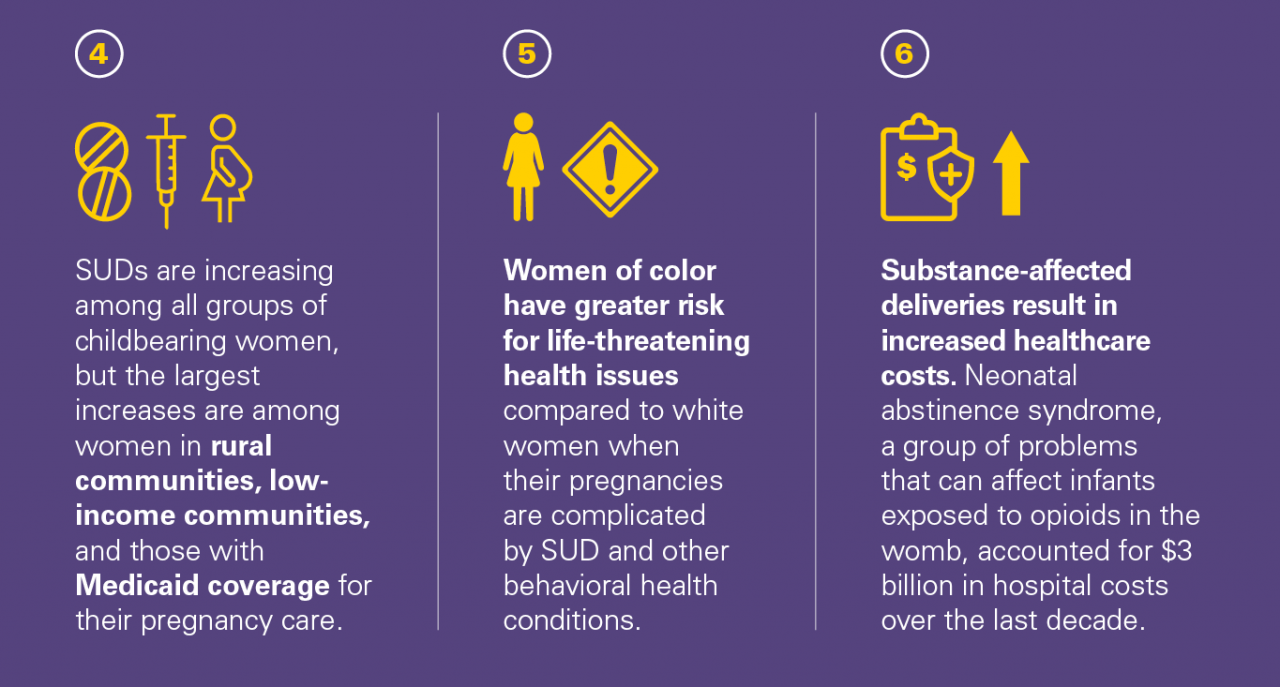
The U.S. is experiencing a significant increase in births affected by substance use disorders (SUDs), particularly opioid or methamphetamine (or meth) use disorder. Untreated SUDs during pregnancy pose increased risks for life-threatening health problems, even death, for mothers and their infants.
April 2019
Takeaways from our research
What does this mean for health policy and practice decisions?
Improving health outcomes for pregnant and postpartum women with SUD requires coordinated clinical and policy-level interventions that are tailored to meet the needs of those at greatest risk.
- Health systems should adopt coordinated evidence-based patient safety practices (bundles) intended to address SUD and racial/ethnic disparities in maternal health. This includes implementing universal screening and referral to treatment for pregnant and postpartum women with SUD.
- Improved quality and availability of local, state, and national surveillance and survey data, specifically linking mothers and newborns, is needed to better understand outcomes after delivery for mothers with SUD and their children, and how to promote continued access to care and long-term recovery.
- Research and clinical guidance on the treatment of methamphetamine use among pregnant and postpartum women is lacking and urgently needed.
Referenced studies on maternal health and substance use by IHPI members
Kozhimannil KB, Admon LK. Structural Factors Shape the Opioid Epidemic’s Effects on Pregnant Women and Infants. JAMA. 2019;321(4):352-353. doi:10.1001/jama.2018.20395
Martin CE, Admon LK, Terplan M. Behavioral Health in Pregnancy and Postpartum: Contributors to Maternal Mortality. Contemporary OBGYN. Dec. 10, 2018. https://www.contemporaryobgyn.net/pregnancy-and-birth/behavioral-healthpregnancy-and-postpartum
Admon LK, Winkelman TNA, Zivin K, Terplan M, Mhyre JM, Dalton VK. Racial and Ethnic Disparities in the Incidence of Severe Maternal Morbidity in the United States, 2012-2015. Obstetrics & Gynecology. 2018; 2018 Nov 1;132(5):1158-66. PMID: 30303912. doi:10.1097/AOG.0000000000002937
Admon LK, Bart G, Kozhimannil KB, Richardson CR, Dalton VK, Winkelman TNA. Amphetamine- and Opioid- Related Births: Incidence, Outcomes, and Costs, United States 2004-2015. AJPHAJPH. 2018;Jan(0):e1-7. PMID: 30496001. doi:10.2105/AJPH.2018.304771
Winkelman TNA, Admon LK, Jennings L, Shippee N, Richardson C, Bart G. Evaluation of Amphetamine-Related Hospitalizations and Associated Clinical Outcomes and Costs in the United States. JAMA Network Open. 2018;1(6):e183758. doi:10.1001/jamanetworkopen.2018.3758
Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW. Incidence and Costs of Neonatal Abstinence Syndrome Among Infants With Medicaid: 2004–2014. Pediatrics. 2018;141(4):e20173520. doi:10.1542/peds.2017-3520
Admon LK, Winkelman TNA, Moniz MH, Davis MM, Heisler M, Dalton VK. Disparities in chronic conditions among women hospitalized for delivery, United States 2005-2014. Obstetrics & Gynecology. 2017; 130(6): 1319-1326. PMID:29112666. doi:10.1097/AOG.0000000000002357
AUTHORS
Lindsay Admon, MD, MSc, University of Michigan
Tyler Winkelman, MD, MS, University of Minnesota/Hennepin Healthcare Research Institute, Former Robert Wood Johnson Foundation Clinical Scholar, University of Michigan
CONTRIBUTORS
Vanessa Dalton, MD, MPH, University of Michigan
FOR MORE INFORMATION
Please contact Eileen Kostanecki, IHPI’s Director of Policy Engagement & External
Relations, at [email protected] or 202-554-0578.
