

Commentary: Increasing screen time during COVID-19 could be harmful to kids’ eyesight
The coronavirus pandemic is remaking the way children learn, and it could have an impact on their eyes.
Shu-Fang Shih, University of Michigan and Olivia Killeen, University of Michigan
The coronavirus pandemic is remaking the way children learn, and it could have an impact on their eyes.
With schools shifting to online lessons at home, children are spending more time in front of computer screens, and many parents are relaxing screen-time rules for TV and video games to keep kids occupied while social distancing. In the midst of the crisis, many children are spending less time playing outdoors.
This combination – more screen time and less outdoor time – may actually harm children’s vision and put them at higher risk of developing myopia, or nearsightedness. That can lead to serious eye problems in the future, including some potentially blinding diseases.
As a health behavioral and policy professor and an ophthalmology resident interested in health promotion and eye care for children, we’re concerned about the impacts of decreased outdoor time and excess screen time on children’s eyes during the COVID-19 pandemic.
What causes myopia?
Scientists are still trying to understand how myopia, or nearsightedness, develops and progresses.
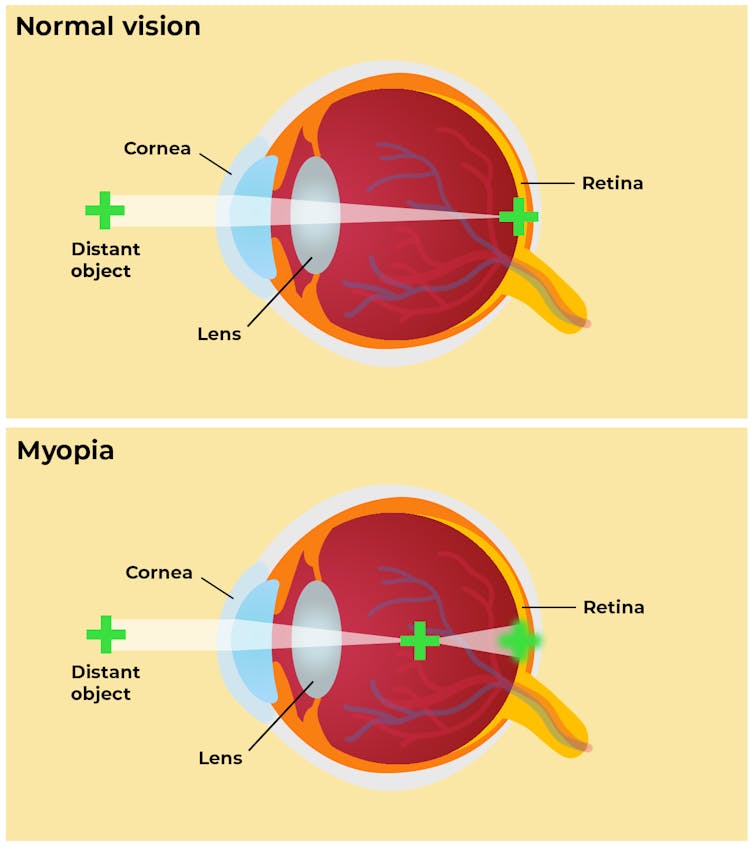
It occurs when the eyeball is too long or the eye’s focusing power is too strong, causing light rays to focus in front of the retina instead of on it, which creates a blurry image. While glasses or contact lenses can correct a child’s vision, research shows that having severe myopia puts children at risk for a number of eye problems down the road, including retinal detachment, glaucoma and macular degeneration.
Some factors in whether a child develops myopia, such as genetics, are beyond a parent’s control, but research shows that other risks can be reduced.
A review of 25 years of research found that working up close – like reading or using a tablet – increased the odds of myopia.
For example, a nationwide study in Taiwan found that after-school study programs with lots of closeup work were associated with an increased likelihood of nearsightedness among children ages 7 to 12. A study of Chinese schoolchildren found that increased time spent working with the eyes focused on something less than 20 centimeters away was associated with myopia. Researchers in Ireland found that greater than three hours of screen time per day increased the odds of myopia in schoolchildren, and investigators in Denmark found that the risk of myopia approximately doubled in Danish teenagers who used screen devices for more than six hours per day.
Getting outdoors matters
Some studies now suggest that spending time outdoors may be able to slow the onset and progression of nearsightedness.
In Taiwan, first-grade students at schools with programs designed to increase their outdoors time to 11 hours or more each week had less progression of myopia over one year compared to their peers. Similarly, in China, researchers found that adding 40 minutes of outdoor activity a day at school reduced the development of nearsightedness in six-year-old children over the next three years.
It is not clear why outdoors time protects against myopia, or why closeup work could make it worse. One theory is that light intensity and time spent outdoors regulates the release of dopamine in the retina, which controls the growth of the eye. Other theories center on how viewing distances impact where the light is focused on the retina; shorter viewing distances indoors may promote abnormal growth of the eye.
Although there is no consensus on how much time children need to spend outside or the importance of the light intensity they are exposed to, it is possible that more outdoor time can help to balance out more closeup work, as a study of children in Australia found.
Childhood is an important time to think about myopia because myopic children tend to become more nearsighted over time. The age of myopia onset is the most significant predictor of severe myopia later in life.
Globally, rates of myopia have been rising. The prevalence of myopia among children ages 6-19 years is estimated at around 40% in Europe and North America, and higher in Asia. By midcentury, researchers studying the trends have estimated that about half the world’s population could be myopic.
Such high rates of myopia also come with an economic burden. The potential lost productivity resulting from myopia was nearly US$250 billion in 2015.
Building an eye-healthy lifestyle at home
Parents can help by carefully managing their children’s screen time to support educational use while limiting cartoons and video games. They can also encourage more outdoors activities while maintaining social distancing.
Having clear rules, setting limits on screen time and parents’ communication style have been associated with less screen time among children. Parental modeling also influences how much time children spend watching TV.
The World Health Organization recommends that children under 5 spend one hour or less per day on digital devices, and children under 1 spend no time on digital devices. The Children’s Eye Foundation recommends daily outdoor play, no screen time for those under age 2, a maximum of 1-2 hours per day for kids ages 2 to 5 and guided screen time with frequent breaks for kids over 5.
Parents and teachers can also check out helpful tips for eye health from the American Academy of Ophthalmology. Educators can find resources to prepare learning materials. Here are some recommendations:
-
Take a 20-second break from closeup work every 20 minutes
-
Set a timer to remind kids to take those breaks
-
Keep digital media 18 to 24 inches away from the face
As we plan the future of education in the age of COVID-19, schools and policymakers must consider children’s vision needs while designing new initiatives. Schools, teachers and parents can work together to incorporate eye health strategies and protect children as they learn online.
Shu-Fang Shih, Research Assistant Professor, Department of Health Management and Policy, School of Public Health, University of Michigan and Olivia Killeen, Resident Physician in Ophthalmology, University of Michigan
This article is republished from The Conversation under a Creative Commons license. Read the original article.
